Bacteria from our own bodies may be responsible for Alzheimer’s – oral bacteria being a prime suspect

A common bacteria found in 75% of adult’s mouths is the likely cause of Alzheimer’s. Frequently called P. Gingivalis, this gram negative, anaerobic bacterium is transmitted through sputum.
You can share it with someone through kissing or sharing eating utensils.
Though new research indicates that a mother passes a majority of her oral bacteria to her baby through the umbilical cord or through the amniotic fluid, P. Gingivalis doesn’t show up until weeks after the baby is born suggesting this periodontal (oral) pathogen is transmitted vertically (likely through mother’s spit). This helps explain the slightly higher risk factor of contracting AD if your mother – not your father – died of Alzheimer’s Disease. This new evidence offers a different explanation to this higher risk. But where it used to solely attributed to genetics, we are now thinking it could be as simple as proximity: as having a mother with this oral bacteria increases the likelihood you’ll contract it from your mother.
Not to worry, many of us live long lives with this bacteria existing in our oral biome because it likes the basic environment of youth and good health. But when both those conditions change, this bacteria causes tissue and bone destruction by convincing your own immune system to turn against you.
How Can an oral bacteria get into the brain?
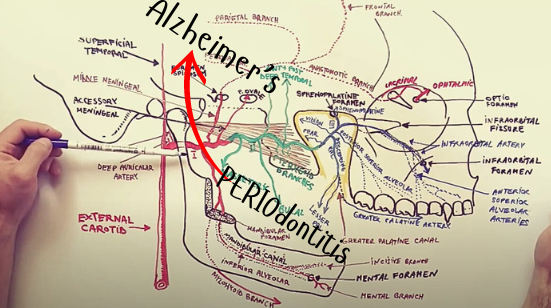
Most Likely Through the Blood Stream
Researchers studying the overwhelming connection between periodontal (gum) disease and Alzheimer’s see that there are three potential ways for oral bacteria to gain access to the brain.
- via the trigeminal nerve
- via the olfactory tract
- via the blood stream, as the main arteries that feed the upper and lower jaws are highways to the interior carotid artery which feeds the temporal lobes of the brain – the hardest and earliest regions to be hit by the tell-tale proteins associated with Alzheimer’s Disease.
How does bacteria survive in the brain?
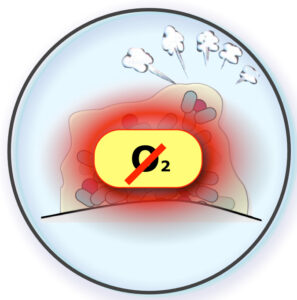
Anaerobic vs. Aerobic Bacteria - NO Oxygen Matters
So this particular bacteria, P. Gingivalis, is quite content in a low or no oxygen environment. Different from the thousands of other common bacterium in the mouth and body that would die in the brain’s vacuum, this one not only can survive, but has a very tricky set of defenses that help it evade the brain’s innate immune system over time.
AD is a Disease of Re-infection, & Re-infection, & Re-infection
Interestingly, researchers are finding lots of cognitively-sound people who don’t have Alzheimer’s Disease at autopsy yet they also have the same protein deposits in their brains.
How is that possible? Why don’t these people show symptoms of AD? Our theory is that the asymptomatic folks that have Amyloid protein deposits experienced a different bacterial infection that was short lived and resolved externally by the administration of systemic antibiotics. The microbe that comes quickly to mind is the bacteria that causes urinary tract infections (UTI). This very common bacterial infection has lots of symptoms and is very detectable by a standard test (culture). As a result, more often than not, the individual who contracts a UTI is placed on antibiotics which halts the infection from continuing to challenge the brain’s own natural defenses. And since the brain uses Amyloid Beta to overtake foreign pathogens that reach the brain, in this situation, there will be Amyloid deposits. And if the glymphatic system (more on that later) isn’t able to clear this debris, the Amyloid stays there indefinitely. The subsequent low bacterial counts of a resolving infection, coupled with the short time the bacteria gets to be in general circulation makes the infection manageable enough for the brain to fight and win.
In this way, we see Amyloid protein as a bit of a CANARY IN THE COAL MINE, in that it signals that a foreign invader had found its way into the brain (and was destroyed/contained/prevented from replicating).
But in the case of diagnosed Alzheimer’s, we see lots more protein – and nearly everywhere throughout the brain. Our theory in this instance is that we are dealing with a different bacterium. A bug, that in the body (the mouth actually) doesn’t create “bell-ringing” symptoms (which is why we still don’t have a test) and is therefore NOT short-lived because it doesn’t get resolved externally by antibiotic dosing. Moreover, with the shear amount of Amyloid build up in AD diseased brains, it stands to reason that the bacteria must be coming from somewhere closer to the brain – like the oral cavity – over an insidiously longer amount of time.
And again, science supports this. The oral cavity is home to over 500 species of bacteria. And the blood supply that feeds your mouth feeds your brain next. Think of it like a train ride where some of these bacterium hop on the blood train in the mouth and rides on into the brain. When we are younger, the bacteria couldn’t get through. But as we age…
And for this reason, the older brain’s immune system is fighting all the time – by itself – losing today, winning tomorrow, only to lose again then next day.
And we see it with our loved one – better today, worse tomorrow, and then spiraling down again. Which is why we refer to AD as a disease of re-infection.
As We Age, Our Brain's Immune System is Breaking Down
Which is why age is the number one risk factor for developing Alzheimer’s Disease. And which is why people who get UTIs when they are young don’t experience psychiatric issues, whereas older people who get this same infection do. The reason for this is simple: the Blood Brain Barrier (BBB), which is our brain’s first line of defense to keep bad things out, becomes less and less effective as we age. The key is a loosening of the “tight junctions” that make up this fortress. Over time, larger and larger particles can get through to the point that something as large as bacteria has an open door. Makes sense why AD is an age related disease – Right?
But Fortunately, There are Things We Can Do to Support our Brain
It’s called Prevention, and we’ve devised a very logical approach to how you can turn the tables on this devastating disease by following some very common sensical rules that will help you live longer and even live better!

